Newsletter (September 2020)
Newsletter (March 2022)
jkld

In This Issue: Life “After” (With) COVID-19
Continuing to Address the Behavioral Health of Coloradans
Supporting our Healthcare Workforce
Investing in our Future
Living with Long COVID: Research and Resources
Collaboration in Action: Supportive Housing for People Experiencing Chronic Homelessness
In This Issue: Life “After” (With) COVID-19
Earlier this month, MHHA marked two years since leaving our office to work remotely, two years since we began facing the devastating challenges of a global pandemic, and two years since we began our “new normal.” If we have learned anything since then, it is that “normal” was already not working for many in our communities. The added stress of the Covid-19 pandemic has made those gaps within our care systems even wider. While the availability of effective vaccines has allowed our state to open back up, the pandemic is still very real for Denverites who are immunocompromised, have limited access to care, are not yet vaccinated, or are too young to receive a vaccination. We continue to brace for new variants while yearning to move beyond. And for those who have lost loved ones and livelihoods, the road ahead is even more challenging.
In February, the Polis administration released “Colorado’s Next Chapter: Our Roadmap to Moving Forward” to outline how our state can prepare for future surges by strengthening our health systems. The administration stresses that “it’s imperative as we transition from the pandemic response into a new chapter where we can use more routine disease control tactics, we not only remain ready if and when something changes, but we build stronger and more resilient systems.”
As we consider the best steps forward, we must seek out the most equitable solutions that will make Denver a healthier place to live for everyone.
Continuing to Address the Behavioral Health of Coloradans
The physical health of Coloradans suffered over the past two years, due to fighting a novel virus and missing needed health care visits, as found by the Colorado Health Institute. As adults and youth have dealt with job loss, financial hardship, unstable housing, social isolation, and increased stress due to the pandemic, behavioral health has worsened for many. This crisis in mental health has disproportionately affected youth and LGBTQ+ individuals in Colorado.
In response, legislators and policy makers have been looking into how to best address this significant need. After the Behavioral Health Transformational Task Force (BHTTF) published their recommendations last month, legislators introduced a handful of behavioral health bills that would distribute COVID relief funds toward residential care facilities and youth supports. Another bill announced this month lays out the structure and responsibilities of Colorado’s new Behavioral Health Administration (BHA), intending to streamline fragmented care and increase access. The Department of Health Care Policy and Financing (HCPF) is also working to improve behavioral health services for Health First Colorado members, and is hosting a stakeholder forum on March 30 about Enhancing Children and Youth Behavioral Health Services. On the local level, through MHHA’s Regional Health Connector, we are working to connect Denverites to culturally relevant community supports and increase social connectedness in order to support mental health and resilience. If you are looking for help, Mental Health Colorado has a list of available resources organized by need.
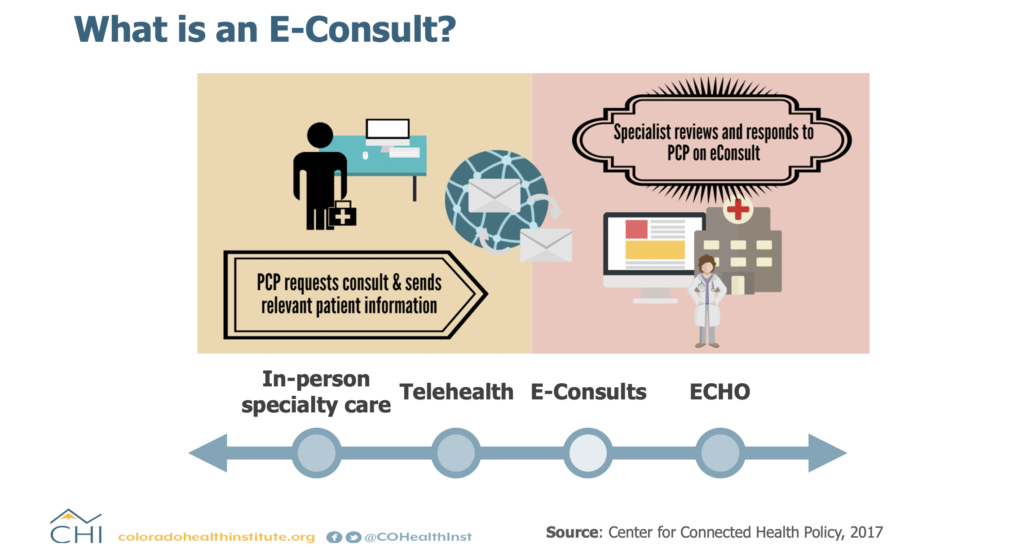
The pandemic also presented an opportunity for advances in telehealth to provide mental health care. Not only does telehealth allow individuals to continue care when staying at home, it also allows expansion of care to those who face transportation challenges or those in rural communities. Telehealth has the potential to increase access to care as long as we consider how to innovate and support this modality equitably. This article from the National Academy for State Health Policy (NASHP) summarizes the lessons learned about telehealth during the pandemic and the questions to consider for the future.
Supporting our Healthcare Workforce
As we plan a healthier future for our state, it is essential that we support the medical professionals, technicians, and first responders who have cared for us throughout this pandemic. We need sufficient and strategic investments in the development and sustainability of our healthcare workforce. Whether through supporting education, lowering licensing fees, or creating more professional pathways, we have the opportunity to expand and diversify those providing care.
In addition to recruiting future workers, we must support those already in the field who have weathered the stress and trauma of the pandemic. Long hours, high case numbers, safety issues and the unrelenting nature of the pandemic have led to burnout among all types of providers. Healthcare Dive reported that Incredible Health found that 34% of the nurses they surveyed planned on leaving their current positions by the end of the year.
HCPF is responding by using American Rescue Plan Act (ARPA) funds to strengthen the Home and Community Based Services workforce. Those interested in providing input on these initiatives can get involved in the Direct Care Workforce Collaborative. Once it is operational, the Behavioral Health Administration will also focus on implementing programs to expand the Behavioral Health workforce. For providers and healthcare staff, ECHO Colorado is offering a six-week series, from April 13-May 18, on coping with the stress and loss of the pandemic.
Investing in our Future
March 11th marked one year since the American Rescue Plan Act was passed. As a result of this pivotal bill, Colorado received $9.7 billion to assist in recovering from the pandemic. This map from the Colorado Health Institute shows how the funding was distributed across state agencies. HCPF has been tasked with investing $501 million in matching federal funds into Home and Community Based Services. See their website to learn more about stakeholder engagement opportunities and to subscribe to regular updates.
Additionally, ARPA funds were designated for other health-related social needs, such as housing, transit, and education. During the current legislative session, the Colorado Sun is tracking what ARPA spending bills are introduced and passed. Last month, the Affordable Housing Task Force released their recommendations, which were based on stakeholder and community member input, to increase access to housing using $400 million in ARPA funds. So far, three bills have been introduced in the state legislature: SB22-160, SB22-159, and HB22-1304, which would direct these funds towards a loan program for resident-owned mobile home communities, a revolving loan program, and grants to local governments and nonprofits.
To track spending, Denver has published a dashboard, now available on the city’s website.
With ARPA dollars for emergency housing assistance still available, the Department of Local Affairs (DOLA) has opened up Emergency Rental Assistance Program (ERAP) funding to those who have not been impacted by COVID-19 but may qualify due to financial hardship. At MHHA, we are continuing to advocate for safe and healthy housing through our involvement in efforts like the Medical-Legal Partnership Community Champions with the Farley Health Policy Center and Renters’ Roundtable, hosted by the Colorado Poverty Law Project.
Living with Long COVID: Research and Resources
Two years into this pandemic, researchers are still trying to understand the causes and effective treatments of “Post-Acute Sequelae of SARS-CoV-2 infection (PASC),” commonly known as long COVID. While so much remains unknown, millions of Americans are experiencing the symptoms of long COVID every day. Symptoms vary from person to person, but the most severe can disrupt people’s lives and work.
This month, the White House released their National COVID-19 Preparedness Plan, which outlines initiatives to expand vaccination access and prepare for future variants. Last year, the Biden-Harris Administration, when recognizing the 31st anniversary of the Americans with Disabilities Act, released guidance that acknowledges that long COVID can be a disability protected by the ADA. The Department of Labor has also gathered Coronavirus resources for workers on their website, including information on how to request workplace accommodations due to long COVID.
Providers can benefit from understanding emerging research and best practices for treating long COVID. In order to study and share findings on long COVID, the Colorado Clinical and Translational Sciences Institute (CCTSI) at CU Anschutz is participating in the RECOVER initiative, organized by NIH. The RECOVER website features resources for providers, including informational webinars and news about ongoing research. Another learning opportunity, offered by the University of Colorado, informs providers about the most recent findings on Post-COVID Conditions (PCC) and Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) through a self-paced course. To view previous recordings or sign up for the course, visit the website here.
Collaboration in Action: Supportive Housing for People Experiencing Chronic Homelessness
In this new section of our newsletter, we are highlighting examples of partnering to improve health. Last September, the U.S. Department of the Treasury awarded a Social Impact Partnership to Pay for Results Act (SIPPRA) Project grant to the City of Denver for the Housing to Health program (H2H). Two MHHA members, the Colorado Coalition for the Homeless and the Mental Health Center of Denver, have partnered with Denver to support this program. See below for a brief description of the program, or read the full press release from the Treasury Department here.
“Denver has developed a Social Impact Bond initiative to ensure the City is paying for the most effective services, “Paying for Success,” and shifting its spending from short-term band-aids to long-term, sustainable solutions. The supportive housing initiative targets chronically homeless individuals who also struggle with mental health and substance abuse challenges. Through local and national partner organizations, the initiative will serve at least 125 chronically homeless individuals over the next seven years using Social Impact Bond financing in combination with existing housing and Medicaid resources. The program will be based upon a proven model that combines the approaches of Housing First with a modified Assertive Community Treatment (ACT) model of intensive case management.”
.