
Newsletter (March 2020)

In This Issue:
All Things Medicaid: Is the Safety-Net Stable?Be Counted – Census 2020
MHHA invited to join MLP Safe and Healthy Housing Cohort
Medicaid and the Coronavirus
“Long-awaited interoperability rules finalized by Trump admin”
(Almost) Welcome Our New VISTA – Tim Morton
ReFUND Colorado – An Easy Way to Support MHHA
All Things Medicaid: Is the Safety-Net Stable?
COVID-19 Update: At the PIAC call on March 18, HCPF Director Kim Bimestefer and Medicaid Director Tracy Johnson spoke about actions the Department is taking to respond to COVID-19. A section 1115 waiver was submitted on Friday, March 13th to CMS including approval for a variety of temporary measures. The 14-page waiver application included 11 amendments to Appendix K, Home and Community Based Services. Changes include:
- Paying telehealth/telemedicine (computer, phone, text, eConsult) at the same rate as for a regular encounter.
- Getting people enrolled in Medicaid quickly; as people lose their jobs they are first filing for unemployment and then Medicaid enrollment.
- Getting providers credentialed including those waiting, graduating, and retired.
CMS has approved a 6.2% FMAP bump over the current 50% rate; HCPF had requested 100% and is still working on it.
With the economic impact of COVID-19, the state revenue forecast will be significantly affected. There is the concern that if we get approval from CMS to make changes, will the state be able to afford it.
There are so many pieces in motion with Medicaid right now that it’s hard to keep up with everything. The issues most on my mind these days are declining enrollment, Payment Error Rate Measurement, the proposed Medicaid Fiscal Accountability Rule, and uncertainty about the Community Health Center Fund.
Through the Medicaid expansion under the Affordable Care Act, along with the “welcome mat” effect, over 100,000 new Medicaid holders were enrolled in Denver, which helped cut our uninsured rate by half. These newly-enrolled have had the opportunity to access regular healthcare, as well as the additional care coordination services provided through Colorado Access, Denver’s Regional Accountable Entity.
As a result of ACA implementation and Medicaid expansion, safety-net providers in Colorado made substantial improvements, increasing services, programs, and even locations to better serve residents who face some of the greatest barriers to gaining coverage and accessing care. However, changes to policy and regulation at the federal level now threaten to undermine Medicaid and destabilize the safety-net in Colorado.
Below is a very brief summary of each of the above topics and, for those of you who want to go deeper, some additional links to further reading. The most important take-away: if we fail to act, the healthcare safety-net could experience a significant contraction, jeopardizing operations at critical facilities and leaving many Coloradans without coverage or care.
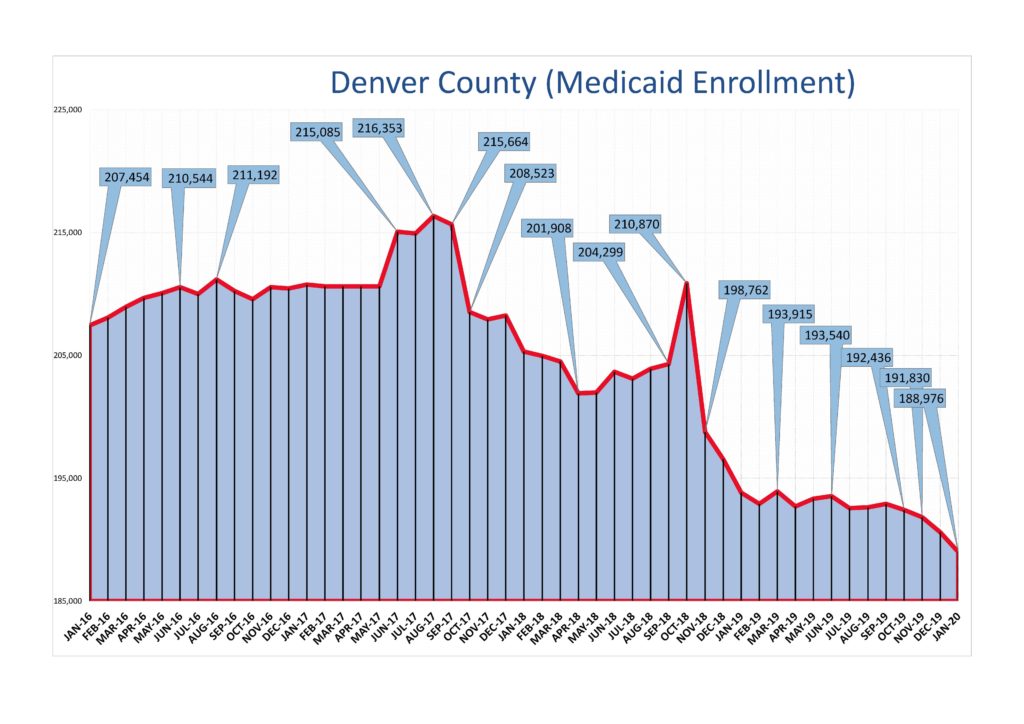
- Decline in Medicaid Enrollment: MHHA has been focused on understanding in more detail the factors contributing to the decline in Medicaid enrollment and rising uninsured rate among our members, with the goal of developing strategies to mitigate the erosion of the payer mix. As the ratio of uninsured to insured patients increases, these facilities have fewer resources to meet the needs of the people they provide care for.
The Colorado Center on Law and Policy released a report in December about the Medicaid decline, outlining several potential factors for decreased enrollment, including a stronger economy, the “chilling effect” of Public Charge, and operational changes made by HCPF in response to pressure from CMS.
MMHA contributed to helping Colorado Health Institute develop a research agenda on declining Medicaid enrollment, and CHI has received funding to proceed with the development of two related reports. The first is due out in April.
What you can do: Let MHHA know if you have experienced declining Medicaid enrollment and how it has affected operations and the people you serve.
- Medicaid Payment Error Rate Measurement: “PERM” measures “improper” payments in Medicaid based on audits of whether a state is implementing its program in accordance with federal and state policies. The Center for Medicaid/Medicare Services has interpreted PERM differently, equating the errors with fraud, and indicating that they may claw back funding from states whose audits reveal an error rate greater than 3%.
At the February meeting of the Program Improvement Advisory Committee for the RAEs, Medicaid Director Tracy Johnson shared that Colorado’s PERM is 28%, putting $30-$60 million or more of Medicaid funding at risk. As a result, HCPF is “implementing several work streams in partnership with county partners to improve eligibility practices.” For now, the claw back remains theoretical, but clearly is driving a number of HCPF’s operational decisions.
What you can do: Work with the counties to ensure people keep their information with HCPF up to date and complete the income verification requirements promptly.
- Medicaid Fiscal Accountability Rule (MFAR): While intensely wonky, this proposed rule by CMS could have a significant impact on financing mechanisms for Medicaid, such as the Hospital Provider Fee. We don’t know what the exact impact of MFAR would be in Colorado, but the Colorado Hospital Association in their comment letter estimated a $3 billion loss in Medicaid funding as a result. To learn more, read Cindy Mann’s excellent blog post.
What you can do: The comment period has closed, so the best course is to contact CMS and ask the rule be withdrawn.
- Community Health Center Fund: Funding for Federally-Qualified Health Centers has been caught up in the federal budget chaos since last summer. Support for the CHCF has been maintained through a series of “Continuing Resolutions,” which is what happens when Congress doesn’t reach an agreement on a new budget by the October 1st start date. CHCF support was extended for 60 days, then 30 days, and then until May 22, 2020. But there is still uncertainty about when and if the federal budget will be passed, and how much will be earmarked for the CHCF.
What you can do: Contact members of Congress to urge full funding of the CHCF.
Be Counted – Census 2020
COVID-19 Update: Mandatory and requested restrictions on gatherings and close contact will have a significant impact on our Census outreach, education, and enrollment efforts. MHHA is developing new strategies, such as phone and direct mail, to substitute for our original outreach plans. If you have ideas about how we can effectively reach hard-to-count populations in these challenging times – or how we could partner with your organization – please email Census2020@milehighhealthalliance.org.
The Mile High Alliance (MHHA) has received three time-limited Census 2020 grants to provided education and outreach for “hard to count” populations in Denver. The funding is designed to offer staff and community education presentations and provide collateral material for MHHA members and community organizations, as requested. The collateral materials are available in English/Spanish and various other languages. Additionally, MHHA will collaborate with various community partners to coordinate five community Census/health events in Southwest Denver and Montbello.
MHHA’s model for Census outreach and education includes the following activities:
- Providing collateral materials for partner organizations that can reach hard-to-count communities in Denver
- Providing Census training for your staff
- Post-training technical assistance if your staff have questions
- Help with the development of a work or action plan for Census plans for your organization
To date, we have facilitated two community presentations/training and have additional presentations scheduled in the upcoming months. We welcome the opportunity to provide additional information and assistance to your organization. Please feel free to contact us at census2020@milehighhealthalliance.org
MHHA invited to join MLP Safe and Healthy Housing Cohort
MHHA was invited to participate in the MLP Safe and Healthy Housing Cohort. By convening this cohort, the Network for Public Health Law (NPHL) and the National Center for Medical-Legal Partnership (NCMLP) aim to support MLPs working at the intersection of individual patient/client needs and population health. The conveners will facilitate opportunities for peer discussion and will provide legal technical assistance to support MLP efforts to improve health through housing.
The NPHL and NCMLP commit to working with the cohort on developing a legal strategy to improve access to safe and healthy housing. The conveners will partner on legal strategy implementation by providing up to 20 hours of legal technical assistance, connecting MLP leadership with state and local health departments, and facilitating three virtual meetings of the cohort. Cohort members will periodically check in with point persons. These meetings will serve as an opportunity to adjust the legal strategy, brainstorm solutions to obstacles, identify new contacts, and celebrate accomplishments to date.
In addition to participating in the cohort, members will attend and engage in three virtual meetings and participate in the 2020 Public Health Law Conference in Baltimore, MD, where the cohort will convene in person.
Medicaid and the Coronavirus
Here is an important discussion of the connection between the current COVID-19 pandemic and Medicaid by Sara Rosenbaum from George Washington University:
“In their recent editorial on the burgeoning public health crisis brought on by the fast-spreading coronavirus, David Blumenthal, M.D., and Sara Collins point out Medicaid’s long-standing role as the nation’s single largest health care first responder. ” [Read more]
“Long-awaited interoperability rules finalized by Trump admin”
“Trump administration healthcare officials on Monday (March 9th) finalized two highly anticipated rules prohibiting the practice of information blocking and giving patients more agency over their medical data. The rules had been held up amid controversy and a fierce industry discussion about patient access versus privacy and security.” [Read more]
(Almost) Welcome Our New VISTA – Tim Morton
We were hoping to onboard our new VISTA on April 13th. However, in response to COVID-19, the Corporation for National Service has delayed all new positions until May.

Tim graduated from CU Boulder last spring with a degree in Integrative Physiology and a minor in Spanish:
“I’ve been aspiring to improve the health of our society since high school and am looking for the best way to make the biggest impact. Working for underserved populations with MHHA is a great way for me to combine my interests in science and research with my passion for community service. Outside of work, I try my best to live an active lifestyle. My hobbies include skiing, ice hockey, and helping my mom train guide dogs.”
ReFUND Colorado – An Easy Way to Support MHHA
If you get a state income tax refund in 2020, you will have a new opportunity to donate some or all of it to support our ongoing work in the community. Since Mile High Health Alliance is a project of the Colorado Nonprofit Development Center (CNDC), all donations will be made using their name and tax ID number.
The new program described by the ReFUND CO initiative puts you in charge of where your donation goes. It’s as simple as 1,2,3:
1. Decide how much of your refund to donate.
2. Enter Colorado Nonprofit Development Center and their registration number 20023005384 in the Donate to a Colorado Nonprofit Fund line on your state income tax return or tax software. NB: In order for these funds to be allocated to Mile High Health Alliance, please use this link to provide information about your donation.
3. Smile knowing you’ve helped a cause that matters to you!
As always, we’re grateful for your past support and hope you’ll consider donating again through this new program to maintain our mission.

Quote: “It’s no longer sufficient to segment the population into those individuals who are most likely to have high costs; we need to segment by those whom we can help in partnership with other sectors, and build those partnerships to ensure their long-term recovery.“
David Labby, MD, MPH, Health Strategy Advisor and former Chief Medical Officer at Health Share of Oregon. [Read more]